Stillbirth risk
My wife is pregnant and due in December. This will be our second child, and everything is going fine so far. With our first child, she didn't have many of the standard pregnancy problems. This time she has swollen feet and ankles, and pregnancy-related carpal tunnel syndrome, and is generally more tired and out of breath. Because I'm a stay-at-home homeschooling dad, it means I hang out with many pregnant women and hear all the intimate and graphic details moms share with each other, and so I know my wife's symptoms fall into the "stuff 99% of pregnant women have" category.
She's gone to all her appointments, and everything checks out fine each time. There are no neural tube defects that can be found, there are no genetic abnormalities the extremely expensive genetic tests could find, the baby is developing normally and is quite active, and mom is doing fine.
So now we're in the 32/33 week area. My wife came back from her latest appointment and said her OB/GYN wants her to come in weekly for biophysical profile (BPP) testing. Oh my god! Was there some problem detected?! Did they find a problem with her or the baby?
No. Nothing has changed: it's still a very good, normal pregnancy. The only reason for the testing is that my wife is classified as "high risk". Because she's 39.
While stillbirth is nothing to take lightly, I knew the risk was small, and less so for someone who's already had a child and has no other risk factors.
After figuring out what the BPP entailed (lots of sonograms and other monitoring/estimating), I decided to take a dive. Here's what I found.
1) The risk is very small
The overall stillbirth rate for women 35-39 is 0.26% (http://www.sciencedirect.com/science/article/pii/S0002937806007435). Some other studies put that number even lower (http://www.biomedcentral.com/1471-2393/13/12). While you'll hear that put as "older women face a 30% increased risk", that's the relative risk, not the absolute risk. A very small risk increased by 30 or 40 percent is still very small.
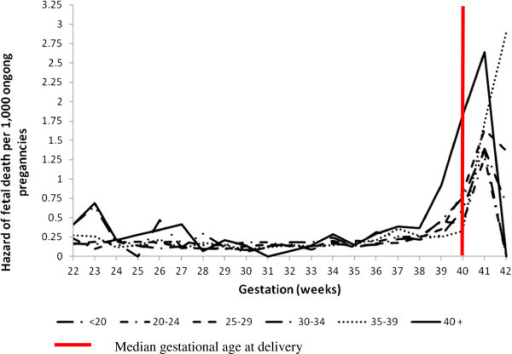
This graph shows the risk per gestational age and maternal age:
 http://openi.nlm.nih.gov/detailedresult.php?img=3552834_1471-2393-13-12-1&req=4
http://openi.nlm.nih.gov/detailedresult.php?img=3552834_1471-2393-13-12-1&req=4
It shows an ongoing risk of about .25 per 1000 for 35-39 year-olds.
Plus, she lacks any other risk factors.
- Previous vaginal delivery.
- Doesn't smoke.
- Doesn't drink or use other drugs.
- Is not obese.
- Is not diabetic.
- No hypertension.
- Overall good health.
I can't find an exact break down of the risk for each factor (in language/terminology I can understand anyway), but the risk is small.
2) The tests (and resulting interventions) don't seem to lower the risk
It's plausible that the tests would detect problems and lead to better outcomes, but do they? From what I can find, there is little evidence that women who undergo the BPP actually have fewer stillbirths:
Biophysical profile for fetal assessment in high risk pregnancies. (http://www.ncbi.nlm.nih.gov/pubmed/18253968 )
"At present, there is insufficient evidence from randomised trials to support the use of BPP as a test of fetal wellbeing in high-risk pregnancies."
"… available evidence from randomised controlled trials does not support the use of BPP as a test of fetal wellbeing in high-risk pregnancies. We found no significant differences between the groups in perinatal deaths or in Apgar score less than seven at five minutes"
And http://www.uptodate.com/contents/the-fetal-biophysical-profile
"Although the use of biophysical testing schemes to monitor high-risk pregnancies has become routine, this practice pattern has evolved with limited high quality scientific data to support its use. Moreover, there are no randomized trials on which to base recommendations for the best initial testing approach for specific types of high-risk pregnancies, the optimal timing of test initiation, the frequency of testing based on test results, conditions that may affect test results, and the effect of gestational age."
So even with testing and the resulting interventions (induction and cesarean), there doesn't seem to be any reduction in stillbirth.
I could find no studies which showed a reduction in stillbirths due to BPP testing.
I'm sure there are many stories of detecting restricted fetal movement or reduced amniotic fluid volume, then an intervention was made and the baby was successfully born. I don't doubt that. But how do we know the intervention made any difference? Maybe that baby was going to be born successfully without the intervention (and, conversely, the babies who were stillborn would not have been saved by the interventions.) That's why we need RCTs so we have something to compare. Does the intervention reduce the stillbirth rate? The above says either "no", or "there's not enough evidence".
3) The tests are not without risk themselves
False positives are possible: the rate is unknown but obviously not non-zero, and potentially significant. 60% of abnormal modified BPP's are false positive (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2771454/?report=classic)
Some parts of the tests are prone to bias and subjectivity (what is restricted fetal movement, how much activity counts, are we looking correctly for AFV, etc).
Sonograms are an unknown risk. While they seem safe, there are some tentative links to developmental problems later. These concerns will probably turn out to be nothing (but in a risk/benefit game, there must be a benefit to justify any risk).
The main risk is that if the test shows something (possibly due to a false positive), an intervention might take place. If the volume seems to be shrinking, they will induce. Pitocin is not without risk and can have pretty serious side effects, and will not work anyway if it's too early, which leaves cesarean, which is even riskier. And, per #2, there doesn't seem to be a benefit to this increased risk.
Conclusion:
The tests haven't shown value, are of significant cost in money, time, and stress (none of which we can afford), and could possibly lead to medically unnecessary (or unproven) interventions.
The risk is very small. Yes, stillbirth is still possible, and that'd be tragic, but it seems extremely likely that even if we did the tests, it wouldn't have prevented the tragedy.
So, if the worst happens and the baby is stillborn, and the doctor starts in with "If only we'd done those tests…", I know what will happen. One: I'll rub my sore knuckles while the insensitive ass regains consciousness. Two: I'll call bullshit. Based on what we know now, the tests would not have offered any protection. All we can do is go on the best evidence we have now.
Further reading:
From "Antenatal Testing – A Reevaluation" ( http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2771454/ )
"As many as 50% of late fetal deaths occur in women without identifiable risk conditions"
"There is little evidence to allay concerns that early onset of antepartum fetal surveillance may lead to situations in which false positive test results lead to inductions of labor, potentially higher cesarean delivery rates, and iatrogenic prematurity."

Comments
_ Add comment